What you’ll learn
- Why patch-based wearable devices for medical monitoring are gaining more research attention.
- How these devices are fabricated to achieve specific objectives.
- How some wearable devices implement monitoring and others add control.
Medical-related electronics research is receiving lots of attention (and funding) due to the confluence of various technical, medical, population, and other factors. How much influence each of these has could be discussed at length without a firm conclusion. But one thing is clear: Much of the work being done, especially in university-related settings, is centered on wearable skin patches that provide different types of functionality.
Why patches? The question should really be “Why not?” They provide a direct way to accomplish various objectives, are relatively easy to monitor, don’t require invasive surgery, and are “student-research” friendly. They are certainly much more easily evaluated and tested than implanted devices, which also accelerates the entire development and evaluation cycle.
The four recent patch-related projects cited here are just a few of the ones that have been recently published. Note that each has a different focus, showing the breadth of patch-related research now underway.
Example #1: Screen-Printed Electrodes
A multi-institutional research effort led by Washington State University has demonstrated electrodes that can be created using just screen printing. The resultant stretchable, durable circuit patterns can be transferred to fabric and worn directly on human skin. In contrast, current commercial manufacturing of wearable electronics requires fairly expensive processes involving clean rooms.
While some other implementations presently use screen printing for parts of the process, this new method relies strictly on screen printing.
They used a multi-step process layering polymers and metal inks to create snake-like structures of the electrode. The screen printing of the polyimide (PI) layer enables facile, low-cost, scalable, high-throughput manufacturing.
PI mixed with poly(ethylene glycol) exhibited a shear-thinning behavior, significantly improving the printability of PI. The premixed Ag/AgCl ink is then used for conductive layer printing. Multiple electrodes are printed onto a pre-treated glass slide, which allows them to be easily peeled off and transferred onto fabric or other material (Fig. 1).
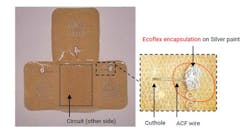
1. For the stretchable, conformable patches, the multistep process involves layering polyimide (PI) and conductive Ag/AgCl inks to create structures of the electrode.
While the resulting thin pattern appears delicate, the electrodes aren’t fragile. The serpentine pattern of the screen-printed electrode accommodates natural deformation under stretching (30%) and bending conditions (180 degrees), which are verified by computational and experimental studies (Fig. 2).
2. This bottom view of the device doesn’t show most of the inner workings (ACF is anisotropic conductive film).
After printing the electrodes, the researchers transferred them onto an adhesive fabric that was then worn directly on the skin by volunteers. The wireless electrodes with on-board associated circuit, including a 2.4-GHz Bluetooth link, accurately recorded heart and respiratory rates, sending the data to a mobile phone (Fig. 3).
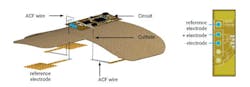
3. An exploded view of the device provides more perspective on the completed arrangement.
In addition to Washington State University, the team included the Georgia Institute of Technology and Pukyong National University in South Korea. The work is detailed in their American Chemical Society (ACS) paper “Fully Screen-Printed PI/PEG Blends Enabled Patternable Electrodes for Scalable Manufacturing of Skin-Conformal, Stretchable, Wearable Electronics,” with more details in the Supporting Information file.
Example #2: Electronic Bandage Speeds Healing
Northwestern University researchers developed a small, flexible, stretchable bandage—claimed to be a first-of-its-kind—that accelerates healing by delivering electrotherapy directly to the wound site. In an animal study, the new bandage healed diabetic ulcers 30% faster than in mice without the bandage. The bandage also actively monitors the healing process and then harmlessly dissolves—electrodes and all—into the body after it is no longer needed.
Injuries can disrupt the body’s normal electrical signals. The researchers wanted to see if electrical stimulation therapy could help close small, stubborn wounds where high glucose levels due to diabetes also thicken capillary walls, slowing blood circulation and making it more difficult for these wounds to heal. By applying electrical stimulation, it restores the body’s normal signals, attracting new cells to migrate to the wound bed.
“Although it’s an electronic device, the active components that interface with the wound bed are entirely resorbable,” said Northwestern’s John A. Rogers, who co-led the study. “As such, the materials disappear naturally after the healing process is complete, thereby avoiding any damage to the tissue that could otherwise be caused by physical extraction.”
The joint team developed a small, flexible bandage that softly wraps around the injury site. One side of the smart regenerative system contains two electrodes: A tiny flower-shaped electrode that sits right on top of the wound bed and a ring-shaped electrode that sits on healthy tissue to surround the entire wound. The other side of the device contains an energy-harvesting coil to power the system and a near-field communication (NFC) system for real-time updates (Fig. 4).
4. Materials and designs of a bioresorbable, wireless, and battery-free electrotherapy system: (a) Schematic illustrations of a transient, wireless, battery-free system for electrotherapy mounted on a wound on the foot (left) and in an enlarged view (right) that highlights the different components. (b) Operational diagram of the entire system (RF, radio frequency; ISO, interconnection system operation; LDO, low-dropout regulator). (c) FEA results of the electric field between the positive (+) and negative (−) electrodes. Scale bar, 3 mm. (d) Schematic illustrations of the mode of use, device on a wound before (i) and after healing (ii), removed by cutting the traces to the anode (iii), partially bioresorbed after a period of therapy (iv), and fully bioresorbed (v). The semitransparent orange color represents the healed skin.
The team also included sensors that can assess how well the wound is healing. The device can be operated remotely without wires. This enables the physician to decide when to apply the electrical stimulation and monitor the wound’s healing progress.
By measuring the resistance of the electrical current across the wound, physicians are able to monitor progress. A gradual decrease of current measurement relates directly to the healing process. So, if the current remains high, then physicians know something is wrong.
In a study of animal models, the researchers applied electrical stimulation for just 30 minutes a day. Even this short amount of time accelerated the closure by 30%. When the wound is healed, the flower-shaped, ultra-thin molybdenum electrode simply dissolves into the body, bypassing the need to retrieve it. Furthermore, it doesn’t interfere with the healing process.
The work is explored in their paper in Science Advances, “Bioresorbable, wireless, and battery-free system for electrotherapy and impedance sensing at wound sites,” which also includes the appended Supplemental Information. Check out this two-minute video:
Example #3: Sweat Sensor with Immediate Readout
Sweat is a “gold mine” of useful information about the body. Recognizing its virtues, engineers at the University of California San Diego developed a thin, flexible, and stretchy sweat sensor that can show the level of glucose, lactate, sodium, or pH of sweat, and do so at the press of a finger.
They claim it’s the first standalone wearable device that allows the sensor to operate independently—without any wired or wireless connection to external devices—to directly visualize the result of the measurement. The design of this small disk-shaped patch includes all of the essential components that are required for wearable sensors: two integrated batteries, a microcontroller, sensors, the circuit, and a stretchable display.
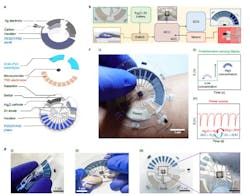
Fabrication of the device involves the formulation of nine types of different stretchable inks, which were used to print the batteries, circuits, display panel, and sensors. The device is printed layer-by-layer onto stretchable polymer sheets and then assembled with hydrogels and microcontroller chips into the complete device. Each ink was optimized to ensure its compatibility with other layers while balancing its electrical, chemical, and mechanical performance (Fig. 5).
5. System overview of the all-printed skin-interfaced ECD sensing patch: (a) Exploded view detailing the individual layers of the epidermal patch. (b) System flowchart of the system and the zoomed-in view of the individual modules. (c) Operation of the patch. Photographic image demonstrates the patch used for epidermal sweat sensing by instantaneously revealing the target concentration (i). Illustration of the change in display that changes with the electrolyte concentration and readout of the potentiometric sensor (ii) and the intermittent discharge mode of the Ag2O–Zn battery that supplies power to the system (iii). (d) Photographic images demonstrating the mechanical performance and durability of the patch, including its bending (i) or stretching (ii) and stretching of the connection between the interconnect and MCU (iii).
Typical electrochromic displays require transparent glass panels with a conductive but brittle coating, which would not work for this device. Instead, the researchers turned to a special polymer called PEDOT:PSS, which is both conductive and has electrochromic properties.
The polymer changes from light sky blue to dark navy blue when applying a negative voltage; it turns back when applying a positive voltage. By tuning the ink formulation with PEDOT:PSS, it can be made both printable and stretchable—the patch can be stretched 20% repeatedly without affecting its performance (Fig. 6).
6. The patch can be stretched 20% repeatedly without affecting its performance.
The researchers designed a display panel composed of 10 individual pixels, which is programmed to display the concentration of the chemicals by turning on different numbers of the pixel. After optimizing the operation condition of the display, each pixel can be turned on and off reversibly over 10,000 cycles, more than sufficient for its week-long operation.
The pixels only take 500 ms to change color, during which time they consume just 80 µW of power on average. As it requires no power to maintain the displayed result, the display is very energy-efficient for its application.
Full details can be found in the Nature Electronics paper “A stretchable epidermal sweat sensing platform with an integrated printed battery and electrochromic display,” which also has appended Supplemental Information.
Example #4: Smart Bandage Promotes, Monitors Healing
A smart bandage developed at the California Institute of Technology (Caltech) may make treatment of wounds that will not go away—and ultimately become infected and fester—be easier, more effective, and less expensive.
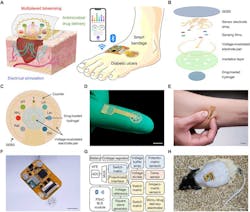
Unlike a typical bandage, which might only consist of layers of absorbent material, the smart bandages are made from a flexible and stretchy polymer containing embedded electronics and medication. The electronics enable the sensor to monitor for molecules like uric acid (UA) or lactate and conditions like pH level or temperature in the wound that may be indicative of inflammation or bacterial infection (Fig. 7).
7. A wireless stretchable wearable bioelectronic system for multiplexed monitoring and treatment of chronic wounds: (A) Schematic of a soft wearable patch on an infected chronic nonhealing wound on a diabetic foot. (B) Schematic of layer assembly of the wearable patch, showing the soft and stretchable SEBS poly[styrene-b-(ethylene-co-butylene)-b-styrene] substrate, the custom-engineered electrochemical biosensor array, a pair of voltage-modulated electrodes for controlled drug release and electrical stimulation, and an anti-inflammatory and antimicrobial drug-loaded electroactive hydrogel layer. (C) Schematic layout of the smart patch consisting of a temperature (T) sensor, pH, ammonium (NH4+), glucose (Glu), lactate (Lac), and UA sensing electrodes; reference (Ref) and counter electrodes; and a pair of voltage-modulated electrodes for controlled drug release and electrical stimulation. (D,E) Photographs of the fingertip-sized stretchable and flexible wearable patch. Scale bars, 1 cm. (F,G) Schematic diagram (F) and photograph (G) of the fully integrated miniaturized wireless wearable patch. Scale bar, 1 cm. (ADC, analog-to-digital converter; AFE, analog front end; PSoC, programmable system-o- chip; MUX, multiplexer; BLE, Bluetooth Low Energy) (H) Photograph of a fully integrated wearable patch on a diabetic rat with an open wound. Scale bar, 2 cm.
The bandage can respond in one of three ways. First, it can transmit the gathered data from the wound wirelessly to a nearby computer, tablet, or smartphone for review by the patient or a medical professional. Second, it can deliver an antibiotic or other medication stored within the bandage directly to the wound site to treat the inflammation and infection. Third, it can apply a low-level electrical field to the wound to stimulate tissue growth, resulting in faster healing.
The wearable patch is mechanically flexible and stretchable. It can also conformally adhere to the skin wound throughout the entire wound healing process, preventing any undesired discomfort or skin irritation. The patch monitors a panel of wound biomarkers, including temperature, pH, ammonium, glucose, lactate, and UA. They were chosen on the basis of their importance in reflecting the infection, metabolic, and inflammatory status of the chronic wounds.
The disposable wearable patch consists of a multimodal biosensor array for simultaneous and multiplexed electrochemical sensing of wound exudate biomarkers, a stimulus-responsive electroactive hydrogel loaded with a dual-function anti-inflammatory and antimicrobial peptide (AMP), and pair of voltage-modulated electrodes for controlled drug release and electrical stimulation.
The multiplexed sensor array patch is fabricated via standard microfabrication protocols on a sacrificial layer of copper followed by transfer printing onto a SEBS (styrene-ethylene-butylene-styrene) thermoplastic elastomer substrate. The serpentine-like design of electronic interconnects, and the highly elastic nature of SEBS, enables high stretchability and resilience of the sensor patch against undesirable physical deformations.
A four-layer flexible printed circuit board (FPCB) measuring 36.5 × 25.5 mm was used, with the sensor patch directly underneath the FPCB accessed through a rectangular cutout (12 × 3.8 mm). The power-management circuitry consists of a magnetic reed switch and a voltage. The electrical stimulation and drug-delivery circuitry used a voltage reference, op-amp square-wave generator circuit, and a switch array. The potentiometric, amperometric, and temperature sensor interface circuitry consists of a voltage buffer array, switch array, voltage divider, and electrochemical analog front end.
A programmable system-on-chip (SoC) Bluetooth Low Energy (BLE) module was used for data processing and wireless communication. The fully integrated wearable device was attached to the mice or rats using 3M double-sided tape and fixed with liquid adhesive to enable strong adhesion, allowing the animals to move freely over a prolonged period.
The work is discussed in their paper “A stretchable wireless wearable bioelectronic system for multiplexed monitoring and combination treatment of infected chronic wounds” published in Nature Communications. The paper is hard to follow due to its stilted, formal tone and heavily skews toward the biochemistry and medical implication rather than the fabrication and electronics. There’s also a 28-page Supplementary Materials file that provides some more details on the device construction and includes a schematic diagram and bill of materials.