A patient’s temperature has long been a primary indicator of illness. But, when the measurement of that temperature is considered in detail, it soon becomes apparent that what may first appear to be a simple concept in reality is far more complex.
Physiologically, the most meaningful definition of a person’s temperature is the temperature of the blood being pumped from the heart. This is truly a core temperature, and the value has importance because blood, essentially at a constant temperature, flows through the large arteries to the lungs and brain.
If a patient is undergoing major surgery anyway, then measuring temperature with a pulmonary artery catheter (PAC) may be called for. A PAC generally includes a very small thermistor temperature probe that is accurate to 0.1°C. This core temperature measurement is as good as it gets. All other methods are approximations from which the real core temperature can only be inferred.
Mercury oral and rectal thermometers have been shown in several studies to be inaccurate.1 Because of the potential for injury and the toxic material used, they have been banned in many areas. In addition to the dangers posed by mercury and broken glass, these thermometers usually were cleaned with an antiseptic and reused, leading to potential spread of infections. Nevertheless, their popularity was well founded given their low cost and relative ease of use.
Electronic thermometers offer several advantages and have largely replaced mercury thermometers. These devices are based on thermistors and provide accurate and fast measurements at low cost.
For professional applications, the thermistor is located in a replaceable plug-on probe. Because thermistors are routinely manufactured to 0.1°C tolerance, the probes are interchangeable and considered disposable. For home use, an even lower cost results from integrating the thermistor and related circuitry in a single plastic case.
Although the new thermometers have eliminated many of the disadvantages of mercury thermometers, they still are used in the same ways. Whether a patient’s temperature is measured sublingually or rectally, the procedure is invasive, inconvenient, and inaccurate. Many studies have confirmed that a large number of factors can contribute to sublingual inaccuracies, among them being mouth breathing, eating, drinking, snoring, and talking.2
Medical temperature sensing is most closely associated with a patient’s temperature, but several related applications also require accurate measurements. Jeff Pile, director of marketing at Quality Thermistor, observed that a substantial need exists for precision temperature datalogging for medical refrigeration such as used to store blood and pharmaceutical products. The company has developed a range of thermistor-based probes, each with an attached 14-bit ADC and USB I/O. DIRECTEMP™ Datalogging Software running on a host PC completes the system.
To improve measurement convenience and accuracy, noninvasive thermometry approaches based on infrared (IR) temperature sensing have been developed. Because the hypothalamus gland is the body’s primary temperature control mechanism and it shares its blood flow with the tympanic membrane, a popular method relies on sensing the temperature of the inner ear.
This is a good idea, and several products have been developed to exploit it. However, the ear canal is not straight. A special manipulation technique must be developed to properly position the thermometer probe. If the positioning is incorrect, the much lower outer-ear temperature may be measured by mistake. A flexible thermistor-based probe also is intended for inner-ear measurement. But like the IR-based probes, it too must be accurately maneuvered and in addition poses a risk of injury when positioned against the tympanic membrane.
An IR-based technique patented by Exergen infers the inner-ear temperature by compensating for the heat loss from the outer ear. Separately, the same technique has been applied to noninvasively estimate the temperature of blood in the temporal artery.
Fiber-optic temperature sensing also has its place in clinical thermometry. Bovie Medical, the manufacturer of Aaron electrosurgery machines, estimates that electrosurgery is used in 80% of operations. Any time this technique is used, there is an associated risk of electrical shock or burns if unintentional grounding paths exist to the patient’s body.3 A conductive temperature probe could form such a path. Optical fibers are completely nonconductive and immune to any amount of EMI that electrosurgery can generate, so they pose no risk and function reliably throughout procedures.
A question submitted to the FDA-sponsored MedSun newsletter summarized the issue: “We are using electrosurgical units (ESUs) with infants in radiant warmers and are concerned that the patient temperature probe used with the radiant warmer might provide an alternate path for the ESU’s radio frequency energy and lead to a burn at the site of the temperature probe. Are there recommendations from ESU or radiant warmer manufacturers about this or any standard of practice that would provide a reference on the subject?”
The newsletter replied, “One of the standards of practice for ESU use is provided by the Association of Perioperative Registered Nurses (AORN). The organization’s “Recommended Practices for Electrosurgery” appears in its Standards, Recommended Practices, and Guidelines (2005). While there is no reference to the use of ESUs with radiant warmers, the guidelines state, ‘Patient monitoring electrodes (e.g., electrocardiogram, oximetry, fetal) should be placed as far away from the surgical site as possible. Alternate pathway burns have been reported at electrocardiogram electrode sites and temperature probe entry sites with ground-referenced electrosurgery units.’ While modern ESUs are not ground-referenced, some older models may be. One should additionally be on the lookout for the radio frequency from the ESU interfering with the temperature regulation of the radiant warmer; in other words, the temperature display may fluctuate when the ESU is activated.”4
Technologies
Thermistor
Figure 1. Assorted Small Thermistors
Courtesy of Cornerstone Sensors
The term thermistor is a blending of thermal and resistor—a device that changes resistance as a function of temperature. Various metallic oxides are combined with binders and fired to form a thermistor. They can have either a positive temperature coefficient (PTC) of resistance or a negative one (NTC), negative being much more common.
Several thermistors are shown with and without leads in Figure 1. The smallest ones measure only a few thousandths of an inch in size, have very fast reaction times, and can be accurate to at least 0.1°C. According to Daniel McGillicuddy, vice president of sales and marketing at Cornerstone Sensors, “There is a new frontier in medicine where surgeons are using controlled localized heat to treat different maladies, including destruction of temperature-sensitive cancer cells. Some thermistor companies offer micro interchangeable NTC thermistors that can be incorporated into a catheter or needle. Such a small probe enhances the surgeon’s ability to control the amount of heat applied to reduce damage to surrounding healthy cells.”
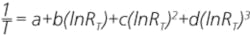
Thermistors are nonlinear devices widely used in all kinds of temperature measurement applications because of their stability, accuracy, and low cost. Nevertheless, being nonlinear, the voltage across them or current through them must be linearized in some way to derive a corresponding temperature. The problem may be appreciated by considering the standard equation many manufacturers use to characterize their thermistors:
where: RT = resistance at the temperature (T)
RT0 = resistance at calibration temperature, usually 0°K or 273.15°C
? = the slope of the thermistor R-T characteristic5
This relationship is accurate at a single temperature but degrades as the temperature span is made larger. An equivalent expression for the R-T characteristic relates 1/T to the natural logarithm of RT. To improve the accuracy of this approximation for larger temperature ranges, Steinhart and Hart, oceanographers at the Woods Hole Oceanographic Institute, proposed linearization via a third-order polynomial:
where: a, b, c, and d = constants measured for a particular thermistor
This equation can linearize temperature measurements based on a thermistor’s resistance to an accuracy between 0.005°C and 0.01°C over a 100°C-span between 0°C to 260°C. Removing the second-order term has very little effect, increasing the error limit to 0.01°C for the same span and range.5
When a thermistor is used to measure temperature, its power dissipation must be kept very low to avoid errors caused by self-heating. In one such application, a thermistor probe is included in a PAC to facilitate thermodilution studies. In this procedure, chilled saline or glucose solution is injected into the right atrium, upstream of the thermistor probe. The temperature difference measured is used to infer probable heart function impairments, a small ?T corresponding to a high rate of flow. In this application, absolute accuracy isn’t as important as high resolution and good repeatability.
Rather than inject cooled fluid, a more modern form of thermodilution applies heat pulses via a second catheter. The heat pulses are accurately and rapidly generated so their position in time is precisely known. In contrast, injecting a chilled solution takes several seconds, and the length of time will vary for each injection. Downstream, temperature is measured by the PAC thermistor and correlated with the heat pulse timing. The method is claimed to be sensitive to 0.02°C temperature differences.6
Several years ago, Yellow Springs Instruments introduced the 400 Series of interchangeable thermistor-based temperature probes, which has become an industry standard. These probes follow a B-series curve with a nominal resistance of 2,252 ? at 25°C. Although the R-T relationship is nonlinear, these probes exhibit a 100-? change in resistance per °C change around 25°C.
David Rowe, product manager for medical consumables and sensors at Philips Healthcare, added, “All Philips temperature probes are Series 400 and EN-12470 compliant. They are accurate to 0.1°C and compatible with patient monitors using Series 400 technology. We have many reusable probes that are autoclavable as well as a range of disposable probes.”
Thermistors also are used in the self-heating mode to indirectly measure airflow. The thermistor’s temperature rise above ambient balances the amount of heat generated by current flowing through the device and heat lost to its surroundings. The corresponding change in resistance is proportional to the cooling effect of the airflow.
This kind of flow sensor must be calibrated to account for different types of anesthesia gases, for example. The same principle is used to measure airflow in sleep apnea machines and patient breathing monitors.
Infrared
When a temperature measurement must be made noninvasively, IR-based instruments may be suitable. Exergen has patented the arterial heat balance (AHB) technique and applied it to outer-ear as well as temporal-artery temperature measurement. By measuring the ambient air temperature and the temperature of the ear or temple area, an estimate of heat loss can be made, and from that, the arterial blood or inner ear temperature inferred.
The company has conducted extensive testing that confirms good agreement between this technique and accepted invasive procedures. In an article describing AHB applied to measure the ear (E) canal temperature (AHBE), the heat-balance proportionality k-factor is discussed: “Specific k-factors programmed into AHBE instrument models vary depending on the site chosen for reference protocols, and are based on extensive published and unpublished clinical data. The calibration is not user accessible, in order to prevent accidental or unauthorized change.”7
Bob Harris, industrial division sales manager at Exergen, explained, “The AHB technology also is used in related applications such as noncontact temperature measurement of fluid being warmed or cooled and transported through disposable tubing. In medical equipment using this technique, AHB provides monitoring or can be the input to a temperature controller.”
An alternative IR approach to patient temperature measurement relies on inserting a probe sufficiently far into the ear canal that at least a partial view of the tympanic membrane is achieved. An article in the Swiss Medical Weekly explored possible measurement impairments such as depth of insertion, obstruction by earwax, environmental acclimatization time, and left or right ear selection.
During tests on the 333 patients included in the study, a wide range of probe insertion depths was measured and various degrees of earwax obstruction encountered. In spite of these conditions, the effect on measured temperature was minimal in all cases.
According to the article, “Neither the mean temperature nor the range of measurements was influenced to a clinically meaningful extent by the depth of penetration of the probe in the external auditory canal. This observation negates our hypothesis that [inaccurate] IR temperature measurement may be associated with… shallow penetration of the probe, assuming a less good angulation of the sensor to the tympanic membrane as compared to deep penetration.”8
Covidien’s tyco Healthcare FirstTemp™ Genius™ instrument used in the study takes 32 measurements as it scans the inner ear during a 2- to 3-second period. At the end of the period, it selects the highest reading as the true value. Oral, rectal, and core temperature offsets can be included in the reported value if required.
During operation, the Exergen device also scans the probe’s field of view, achieved by manually moving the probe as it is held against the outer ear. The highest temperature is selected from 10 taken during a 1-second period. It is this temperature that the Exergen algorithms operate upon to deliver the IR arterial temperature value.
Optical Fiber
A few distinct technologies are lumped together under the term optical fiber temperature measurement. The Bragg grating approach uses a specially prepared fiber to measure temperature. Most other methods transmit light to and from a sensor located at the end of the fiber, and it’s the tiny sensor that does the actual measuring.
A Bragg grating is a periodic physical change in a fiber’s index of refraction that is created by a special manufacturing process. The light frequencies affected by the destructive/constructive interference within this structure change with temperature. By illuminating a Bragg grating and analyzing the reflected light, the temperature of the grating can be determined.
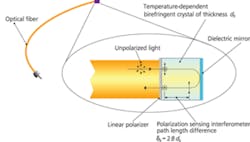
Figure 2. Operating Principle of Birefringence-Based
Optical Fiber Temperature Sensing
Courtesy of Opsens
Opsens uses two different technologies in its fiber-based medical temperature sensors. The company has patented a white-light polarization interferometry (WLPI) method that is used to measure the difference in path length caused by temperature-sensitive birefringence. In this technique, described in Figure 2, a small crystal of a selected material is sandwiched between a linear polarizer and a dielectric mirror to form a two-beam polarization interferometer.
The crystal is attached to the end of an optical fiber that transmits white light to it and couples the reflected light back to a WLPI signal-conditioning instrument. Changes in path length through the crystal primarily depend on the temperature-induced changes in its birefringence, and the signal-conditioning instrument recovers this information from the reflected light. This approach allows various types of crystals to be used depending on the accuracy and temperature span required.9
Opsens and several other companies separately have developed GaAs-based optical-fiber sensors that exploit temperature-induced band-gap changes. As with the WLPI sensor, the GaAs crystal is attached to the end of an optical fiber. Light frequencies corresponding to energies less than the band gap are absorbed, and those greater are transmitted. By analyzing the light reflected from such a sensor, its temperature can be determined.
Both the WLPI and GaAs sensors are ideal for very long-term monitoring because they don’t drift. The parameter being used is a characteristic of the material and inherently stable. Medical applications have time scales from hours to months.
For the medical clinician, optical-fiber-based temperature measurement provides a solution to the safety risks associated with electrosurgery. An ESU cuts by vaporizing the tissue in the immediate vicinity of a probe. RF at frequencies from 300 kHz to 3 MHz and amplitudes from 200 V to 10 kV is generated to accomplish this, and the potential for unintentional patient damage exists any time an ESU is used.10 Fiber-optic temperature sensing is nonconductive and immune to EMI so it can be attached to the patient as required and relied upon during ESU procedures.
Further Considerations
Measurement accuracy always is important when a parameter’s value must lie within prescribed limits. Is there cause for concern if the measured temperature is 0.1°C below the upper limit? How about 1°C above it? If the thermometer itself has a 1°C error, how can you decide which values are critical?
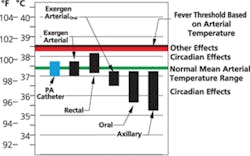
Figure 3. Range of Typical Measurements at Various
Sites Based on 37.4°C Arterial Temperature
Courtesy of Exergen
The picture is further complicated by considering that although Wunderlich’s 1861 report established 37°C as the mean body temperature, it also demonstrated a range from 36.25°C to 37.5°C as being normal.11 In addition, the temperature offsets inherent among sublingual, rectal, and PAC measurements can account for 0.4°C to 0.5°C inconsistencies.12 And, diurnal variation contributes as much as 0.5°C further uncertainty.13
The relationships among the various site-specific values and the typical upper and lower trigger points leading to further investigation are shown in Figure 3. Obviously, a patient’s temperature should be represented as a range rather than a single number. However, this implies an even greater need to minimize measurement error.
Conclusion
Fortunately, modern thermistor manufacturing techniques allow ±0.1°C device matching at low cost, making practical thermometers that are accurate and disposable. Most clinical temperature measurements are made with thermometers based on thermistor technology.
However, both IR and fiber-optic technologies also are important, offering advantages under certain circumstances. IR is noninvasive and can be very accurate. Exergen’s IR thermometers claim to have the added benefit of eliminating the careful positioning associated with other IR products that measure the inner-ear temperature. And, fiber-optic thermometry is immune to EMI, a big plus in electrosurgery.
Regardless of the measurement technology used, it’s clear from the large variation shown in Figure 3 that a patient’s temperature is just one input to a meaningful diagnosis, although an important one. Many other contributing factors also must be taken into account, which underscores the value of thorough clinician training and extensive experience. Nevertheless, an accurate temperature measurement provides reliable guidance for further treatment decisions.
References
- Pompei, M., “Temperature Assessment Via the Temporal Artery: Validation of a New Method,” Exergen Clinical Study, 1999, p. 36.
- Pompei, p. 32.
- McCauley, G., “Understanding Electrosurgery,” Bovie Medical, 2010, p. 4.
- “DS-X Lessons Learned,” MedSun, U.S. Department of Health and Human Services, FDA, Newsletter #4, May 2006, http://www.accessdata.fda.gov/scripts/cdrh/cfdocs/medsun/news/newsletter.cfm?news=4
- “NTC Thermistors,” http://www.thermometrics.com/assets/images/ntcnotes.pdf
- “Continuous Cardiac Output,” Slideshow, Edwards Lifesciences, slide 39, 2003, http://ht.edwards.com/presentationvideos/powerpointslides/cco/cco_speaker_notes.pdf
- Pompei, p. 13.
- Twerenbold, R. et al, “Limitations of Infrared Ear Temperature Measurement in Clinical Practice,” Swiss Medical Weekly, 140:w13131, 2010, p. E4.
- “White-Light Polarization Interferometry Technology,” Opsens, http://www.opsens.com/pdf/WLPIREV2.3.pdf
- Hausner, K., “All Electrosurgical Units Are Not Created Equal,” http://www.elmed.com/Electrosurgery/Info/equal.htm
- Kelly, G., “Body Temperature Variability : A Review of the History of Body Temperature and Its Variability Due to Site Selection, Biological Rhythms, Fitness, and Aging,” Alternative Medicine Review, December 2006
- Pompei, p. 13.
- Twerenbold, p. E5.
| FOR MORE INFORMATION | Click below | |
| Bovie Medical Corporation | Aaron ESUs | Click here |
| Cornerstone Sensors | Small Thermistors | Click here |
| Exergen | Temporal Artery Temperature Measurement | Click here |
| Covidien | FirstTemp Genius | Click here |
| Opsens | Optical Fiber Temperature Measurement | Click here |
| Philips Healthcare | Series 400 Temperature Probes | Click here |
| Quality Thermistor | DIRECTEMP USB Probes | Click here |