2019 Special Report: Telemetry, digitalization driving change in medical test
Download this article in .PDF format.
Of all the applications for electronic test & measurement, none have anything close to the direct impact on the health and well-being of consumers as in medical test. The stakes couldn’t be higher when it comes to the protocols that go into testing electronic medical devices, as the consumer-applications for this field couldn’t be more literal.
Unfortunately for the medical device market, the biggest news that comes from it is often bad: devices causing injury, malfunctions resulting in wrongful death lawsuits, or simply devices not functioning as intended. What’s often lost through the reporting of all the bad that can result from oversights in medical testing is that millions of lives have been saved or made better thanks to medical devices. Nonetheless, it seems device manufacturers are constantly challenged to make sure they stay out of negative headlines. They do so, in large part, thanks to the products and solutions from test & measurement vendors.
Trending
Technological advances in electronic medical test continue to enable engineers to innovate new medical equipment and devices from those used in an emergency room, to wearable devices that allow patients and everyday consumers to monitor specific health factors by checking an app on their smartphone.
We at Evaluation Engineering gathered commentary from several leading test & measurement vendors about what they’re seeing as key recent trends in the area of electronic medical test, or trends they’re expecting to rise in the near future.
Montreal, Quebec-based Averna Technologies, a provider of automated test and quality solutions, elaborated on procedures that go into testing of specific electronic medical devices. Company chief operations officer François Rainville and sales manager Javier Olea combined to pick the incorporation of telemetry into medical devices such as the top trend they’re paying attention to.
“Medical devices that incorporate telemetry features—such as pacemakers, deep brain stimulation systems, insulin pumps, or ventricular assist devices—used to leverage custom protocols to exchange data with medical equipment, devices, or professionals,” Rainville and Olea said. “The reason why medtech companies used custom protocols was for safety reasons, power consumption, and compliance. But now, as commercial technologies become more available, stable, and consume less power, med device companies are relying more and more on technologies like Bluetooth Low Energy (BLE) for their telemetry features. With off-the-shelf connectivity technologies, the development cycle is faster, and from a reliability and compliance point of view, BLE is no longer a concern.”
The Averna duo went on to say that with commercial technologies comes the challenge of safety—specifically in that companies must ensure that unauthorized intrusion is not possible, doing so through incorporating safety features into these standard communication protocols.
“As medical devices integrate more RF and telemetry connectivity features, new test and compliance strategies are required,” Rainville and Olea added. “Consequently, many medtech companies partner with RF test experts to create and implement the appropriate test and compliance strategies at both the R&D and manufacturing stages.”
As another trend, Rainville and Olea said that for pharmaceutical companies, the actual medicine is no longer the only differentiator.
“Now, companies are developing smart injectors that can give real-time insight to medical professionals or administer automatically precise doses,” they explained. “Another technological breakthrough in this industry is the microelectronics pills or capsules that collect and share information and data.”
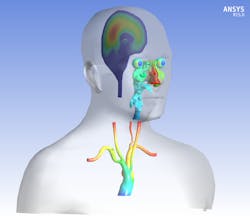
Thierry Marchal, global industry director for healthcare at ANSYS and secretary general of the Avicenna Alliance, stressed to EE that the biggest trend he’s seen in medical device test is the rapid increase in digitalization.
“Computer models are becoming increasingly popular in the medical device industry,” Marchal said. “As they become very accurate and reliable in their prediction of the behavior of any medical device interacting with the human body, they have been used by all leading medical device companies for more than a decade to design and optimize new prototypes. Recently, the FDA, followed by the House of Congress and the US Senate, have paid more attention to this in silico approach (e.g. using computer models to complement the in vitro and in vivo approach).”
Marchal explained that the U.S. Food and Drug Administration (FDA) has been investigating the in silico approach since 2011 and is now strongly encouraging the adoption of this technology by medical device companies.
“After a very successful meeting between Sen. T. Cochran, the FDA, and leaders of the Avicenna Alliance including ANSYS, Medtronic, Johnson and Johnson, etc. in May 2017, the U.S. Senate and House of Congress published bills in July 2017 stating the value of the in silico approach to reduce the risk for the patient but also to reduce the cost of healthcare while accelerating the pace of medical device innovation. As a result, the U.S. Government will be providing funding to the FDA as part of its 2019 budget to support FDA’s in silico and digital twin initiatives."
Marchal added that the European Parliament has similarly agreed to support the development of silico medicine in an event this past September. And this past Nov. 8, the American Society of Mechanical Engineers published a new standard—V&V 40—explaining how to properly verify & validate computer mod-els targeting medical devices so that they could be used for regulatory approval.
“This is opening the door to ‘in silico clinical trial’, e.g. complementing and partially replacing clinical trial by virtual patients and computer models,” Marchal said. “This progressive digitalization of the medical testing is probably one of the most important medical evolution of the last few decades."
Into use
We asked our report respondents to describe a recently completed project that addressed a medical application, the short-comings it addressed, and the key challenges involved. Here’s what they had to say.
Rainville and Olea, Averna: “Great advances have been made recently in both the functionality and size of hearing aids and related accessories. As the devices get ever smaller, they also become ever more powerful with additional functionality and user options. But the trend of miniaturization brings with it multiple new challenges for product designers. That’s why our client contacted Averna—to develop a flexible test solution for RF performance at the physical channel level, ensuring their Bluetooth LE-enabled devices conformed to design specifications. As well, they tasked Averna to architect the test system so it could easily be adapted for other purposes. In other words, they wanted to maximize their return on investment with a future-proof test solution for their evolving product line.”
A universal tester containing all required hardware, including National Instruments’ PXI, PC, and power supply—neatly stored in a standard rack
An expandable fixture on which two PCBAs can be placed at the same time
A mechanical adapter that allows the operator to smoothly change the fixture to hold different types of products
A suite of productivity tools for test sequencing, test data management, system calibration, user management, and other tasks
Marchal, ANSYS: “During a recent event in Brussels, Belgium, Michael Hill, vice president of science, technology, and clinical affairs at Medtronic, illustrated the concrete impact of modelling and simulation on providing regulatory evidence by mentioning one of their products—a pacemaker, recently released two years earlier than expected, reducing the clinical trials by 256 patients and the estimated cost by $10 million while allowing to treat 10,000 patients during these two years. Medtonic is using ANSYS tools among others to test the electromagnetic interaction of implants and human body to avoid local necrosis of soft tissue.
“On one end, there is a strong public opinion and requests from governments all around the planet to minimize the risk for the patients by maximizing the number of tests on larger samples of the target population before approving the release of any new medical product. On the other end, considering that the cost of clinical trial could be up to $40,000 per patient participating to the trial, if regulatory authorities require that medical device companies must increase their clinical trials by thousands of additional patients to better validate the full safety of a device despite the population variability, this request would dramatically increase the cost of the regulatory approval process.
“The use of virtual patients and computer models in a first step, and patient digital twin in a second step, provide medical device companies the opportunity to complement, anticipate, and partially replace traditional clinical trials with ‘in silico clinical trial’—bridging the gap between patient safety on one end, and affordable and profitable healthcare on the other.
“These computer models remain models, a representation of the reality. Therefore, it is crucial to make sure that medical device designers could rely on them before making any medical decision. Technically speaking, it is important for companies to develop reliable models able to accurately predict what is likely to happen in the very complex human body. This never-ending challenge requires more research and investment to improve the models in their accuracy, long-term predictability, and ensure we fully understand the limitations of the current model.
“Validating the models is the second challenge. During the last few years—under the guidance of the FDA and ASME—ANSYS has collaborated closely with the leading medical device companies to develop the new standards for verification and validation of medical devices (ASME V&V 40). Finally, making sure that these models are accepted by regulatory authorities and clinicians is the third challenge requesting a lot of communication and education.”
When things go wrong
This past December, the International Consortium of Investigative Journalists (ICIJ) released the results of a yearlong investigation into the harm caused by poorly-tested medical implants.(1) The findings were led by FDA data showing that more than 80,000 deaths and 1.7 million injuries were possibly linked to medical devices in the 10-year span between 2008 and 2017. It should be noted that the data covered implants of all types—from hip implants to breast implants—and didn’t show results specially for electronic implants.
ICIJ’s research found that in the U.S., the average time for a new device to be approved through the FDA’s premarket approval process has dropped by more than 200 days since 1996. While that major time-to-market improvement is great news for device manufacturers, speeding up the approval process can also result in devices that are more prone to faults. Manufacturers certainly don’t like over-regulation, but minimal testing for the sake of faster marketing often spells disaster, no matter the industry. ICIJ pointed to a 2016 study by medical journal BMJ that found devices first approved in the European Union—known for light-touch regulations—were associated with a higher rate of safety alerts and recalls than those approved in the U.S.
In 2017, Market Research Engine forecasted that market for electronic medical device implants—also known as active implantable medical devices—was expected to exceed $256.75 billion by 2022.(2)
References:
(1) International Consortium of Investigative Journalists, “Everything You Need to Know About the Implant Files,” December 3, 2018.
(2) Market Research Engine, “Active Implantable Medical Devices Market by Product Segment Analysis,” May 2017.
About the Author