Wireless health to drive a trillion sensors
Healthcare is a basic human need; this need is universal and endless. Society expects quality care affordably accessible to all. As in any engineering problem, trade-offs are inescapable in solutions to meeting these expectations. Nevertheless, we would like to believe that quality, reach, and cost should each be optimized without compromises to one another. At the same time, the unending universality of the need makes delivery of healthcare a great business opportunity. The regulatory requirements benefit the incumbents of the industry and provide pricing power.
The U.S. healthcare system is built on fee-for-service, wherein the service is reactive to illness. An aging population, longer lives, and increasing cases of chronic diseases are some of the key drivers escalating healthcare expenditures. Annual U.S. healthcare spending is projected to be ~$3.3 trillion in 2015; that is, ~$10,000 per person. Spending as a share of the GDP generally has remained stable in recent years, at ~18%. Approximately 75% of healthcare cost is associated with chronic diseases (for example, hypertension, obesity, diabetes, asthma, chronic obstructive pulmonary disease, heart failure). Approximately 45% of the U.S. population has at least one chronic disease; about 50% of the population has two or more.
The microelectronics industry, driven by Moore’s law, seems to succeed in continuously making things better, faster, and cheaper. It is tempting, then, to envision the microelectronics-enabled capabilities to bring the same benefits to healthcare delivery as they have to the delivery of many other services (shopping, entertainment, transportation, education, etc.). One such solution is wireless health, which in slight variations also is known as digital health and mobile health (mHealth). The basic idea is to monitor patients remotely while they go about their lives and deliver responsive care preventatively and on demand. Keeping chronic-disease patients out of clinics and hospitals saves care cost. At the same time, there is the prospect of improving quality and reach of care.
Wireless health
Wireless health solutions are enabled by the convergence of four pervasive technologies, namely unobtrusive sensing, wireless communication, ubiquitous computing, and social networking. Miniature, low-cost, high-performance sensors—based on microsystems technology—that can measure a variety of physical, chemical, and biological parameters are increasingly available. These sensors may be worn on the body, implanted in the body, and/or deployed in one’s surroundings; in fact, the typical smartphone continues to incorporate more sensors to better interface with the physical world.
Wireless connectivity is increasingly available with higher performance at lower cost and in smaller form factor and with lower power. From embedded microprocessors to cellular phones to servers in data centers (that is, the cloud), computing is a readily available commodity. Finally, a variety of web-based platforms provides the opportunity to build a wide range of social networks for many different purposes.
The wireless health field is in its infancy and not yet a formal discipline. At this time, it is mostly a concept, but a remarkably powerful and rich one that enables effective and efficient ways to collect, forward, and process medical data and information within the healthcare ecosystem. In the illustration, it is not difficult to imagine “them” to be all elements of the healthcare delivery infrastructure, “me” the consumer patient, “you” my support social network (family, friends, and peers), “him” the care coordinator, and “her” consumer health and wellness companies. This wirelessly enabled ecosystem is a rich resource for care delivery, which can be preventative and personalized as well. In this ecosystem, the consumer patients can be more cared for than ever before while going about their normal lives.
From sensors to wearables to wireless health
Sensors make up the front line of collecting data from the physical world, including our bodies. Wearables such as patches, fitness trackers, smart watches, and smart apparel are enabling platforms that carry sensors, locally process and store onboard sensor data, and transmit this data to off-board computational platforms for further analysis and use. Sensors are, therefore, key to enabling wearables—they are an integral part of wearable technology. A recent study1 predicts that sensors will support a $75 billion wearables technology market by 2025. It forecasts 3 billion wearable sensors by 2025, with about one-third being new sensor types.
Health and wellness applications currently are the major drivers of wearables—the killer applications, no pun intended! While many health applications may require implantable medical devices—often also enabled by sensors—wearable devices are preferable since they are nonintrusive in comparison. In some cases, health and wellness applications may be addressable by “deployables,” devices that are in our immediate environment rather than on or in our bodies. An example is commercial devices on the market deployed under a mattress for sleep monitoring.
Another recent study2 predicts double-digit growth in the next several years in the number of Americans with wearable devices and expects 39.5 million Americans to be wearing fitness trackers and smart watches in 2015—an increase of ~58% from 2014. The study reports that wearables currently are most popular among American adults between 25 and 44. It is natural to expect that use of wearables will grow in popularity among the elderly in support of independent living.
Topol3 provides a list of the top chronic diseases in the United States and the sensors the patients need in each case to monitor their status for a “healthier normal.” Applications are plentiful, but we are technology limited.
Engineers are key to solving care quality, reach, and cost challenges through wireless health solutions. However, they need to work closely with clinicians to assure relevance and efficacy of such solutions. This, in turn, requires becoming familiar with clinical terminology and healthcare delivery ecosystems. An area of importance is user-experience engineering since wireless health devices often closely interact with the user. This area requires specific attention to the user-base needs and preferences. The elderly may not welcome mainstream solutions—consider eyesight and activity differences, for example.
Wireless health products, businesses, and business models
Wireless health product and service opportunities span a wide spectrum of health and wellness needs. They also enable development and deployment of new business models. Although the approach is rooted in basic and feature phones, the rapid growth of the smartphone has played a defining role in turbocharging wireless health innovation. A variety of external sensors can be used in association with a smartphone to expand the range of the wireless health application space. These sensors leverage the phone’s platform and use its capabilities to deliver specific data measurements.
Custom platforms were necessary before the proliferation of smartphones and still may be needed in some applications. However, any project should carefully weigh the application requirements to assess if a custom platform is competitive in the long run. Smartphones advance at a rapid pace characterized by customer receptivity for new features and capabilities. As a result, a custom solution that is unique today may not be competitive tomorrow as the smartphone platform integrates more capabilities.
A point of note in wireless health innovation is that wireless enablement should be a genuine benefit, not just a feature. The wireless enablement is not always necessary; application requirements should be assessed carefully. A given wearable application may be satisfied by collecting and storing data for a period of time, then downloading the data at a docking station.
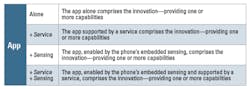
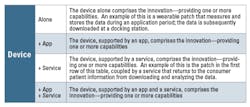
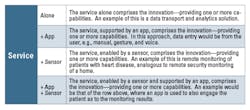
Table 1 outlines the basic approaches to app-driven solutions. Table 2 and Table 3 do the same for device- and service-driven solutions. Since the external devices usually are sensors, the terms sensor and device are used interchangeably here. Focusing on solutions enabled by external devices is not exclusive of also using the phone’s embedded sensors. It should be noted that external devices may be peripherals, such as biometric data routers, usually facilitating the transmission of data from sensors. In Tables 1, 2, and 3, descriptive examples are provided for approaches that may be harder to grasp.
Apps may originate from payers, providers, and/or third parties. Providers are increasingly branding their own apps to engage their patients and enhance their services. Inevitably, these provider apps will tie into the provider’s electronic records, providing access to the patients. Payer apps enhance external-facing service enhancements for both patients and providers. Third-party apps may be for payers, providers, and patients to provide tools that facilitate a variety of workflow, engagement, and care delivery needs.
External sensors may be placed in the body (implantable), on the body (wearable), and off the body (deployable). Implantable devices are the least attractive as they require intrusion into the body, which also substantially increases the technology burden including biocompatibility, power, packaging, and more. However, some applications—such as heart failure and aneurisms—may require implantable pressure sensing. Wearables are comparatively attractive if they do not compromise the wearer’s look and feel. Off-the-body sensors are most attractive when possible, since they do not burden the patient.
Apps, products, and services intended for healthcare (and even consumer health) must consider the regulatory policies and regulations. The requirement for approval from the Food and Drug Administration may not always be obvious, in part because technology advances are outpacing the existing review and approval time constants. At the same time, consumers and patients expect to use the latest available technology capabilities.
Conclusion
The convergence of pervasive technology—sensing, connectivity, computing, and social networks—is enabling care to the patient in the patient’s environment. Providing care is moving from a fixed time and place to anywhere, anytime. Sensors play a key role in this enablement; they capture the data necessary for diagnostics and care decisions, which may be communicated to the patient, patient-specific devices, and the patient’s social network. These new technological capabilities bring about opportunities for new business models centered on devices, apps, and/or services. The potential is great; so are the business opportunities.
References
- Hayward, J., and Chansin, Dr. G., “Wearable Sensors 2015-2025: Market Forecasts, Technologies, Players, “IDTechEx.
- “Wearable Usage Will Grow by Nearly 60% This Year,” eMarketer, Oct. 28, 2015.
- Topol, E., “Transforming Medicine via Digital Innovation,” Science Translational Medicine, Vol. 2, Issue 16, January 2010.
About the author
Dr. Mehran Mehregany is the director of Case School of Engineering San Diego and Veale Professor of Wireless Health Innovation and the Goodrich Professor of Engineering Innovation at Case Western Reserve University. He founded the Case School of Engineering San Diego in July 2007 and its Wireless Health and Wearable Computing programs in 2011 and 2014, respectively. Mehregany has more than 360 publications describing his work with sensors, MEMS, and SiC; holds 20 U.S. patents; is the recipient of a number of awards/honors; and has founded several technology startups.
A wireless health solution example
Pregnancy is a sensitive period in the life of the family. There are a variety of diagnostics that must be performed to track the health of the mother and the baby. One of these diagnostics is to simultaneously monitor contractions and fetal heart rate—more specifically, to determine whether the fetal heart rate recovers normally once a contraction ends. This diagnostic becomes particularly important when the mother and/or the baby face health risks, in which case more periodic or continuous monitoring is desirable.
© AirStrip Technologies. All rights reserved
A wireless health solution that allows this testing at home, with the data forwarded to a clinic, is ideal—not just for risk pregnancies. In developing countries and often remote areas of a developed country, a clinic may be a fair distance away, requiring the mother to travel for the test, often on foot for a few miles. Sometimes, the test is not conclusive, and the mother has to return the next day.
This need drew the attention of Dr. Mehregany while attending the mHealth Summit in Washington, D.C. in December 2009. At the time, he was on leave from Case Western Reserve University, spending a short stint at the West Health Institute (then West Wireless Health Institute) as its founding executive vice president of engineering.
At the institute, Dr. Mehregany and his colleagues, Drs. Enrique Saldivar, Srinivas Ragavan, and Masoud Roham, designed and demonstrated a solution— dubbed Sense4Baby—that included wearable contraction and fetal heart-rate sensors. The sensors were on a belt that the mother could wear around her waist, positioning the sensors on her belly. A Bluetooth radio transmitted the data from the sensors to a necklace the mother wore, which incorporated a broadband radio for transmitting data to a clinic. The necklace was used to position the broadband radio away from the mother’s belly.
The institute continued work on Sense4Baby, creating a final product that was acquired by AirStrip Technologies. AirStrip Technologies subsequently partnered with Apple to develop an app for the iWatch, bringing Sense4Baby to the mass market.1 A demonstration of the AirStrip/Apple solution can be found in the early minutes of the video recording of Apple’s Sept. 9, 2015 Special Event.2
References
- Wicklund, E., “Latest Apple Watch tuned for home health monitoring,” mHealthNews, Sept. 9, 2015.
- Apple Special Event Video, Sept. 9, 2015.